Have you ever experienced a meal where something “went down the wrong pipe”? If so, you’ve experienced what’s known as aspiration. This is a fairly common occurrence that can occasionally lead to aspiration pneumonia when someone can’t cough up whatever has entered his or her airways.
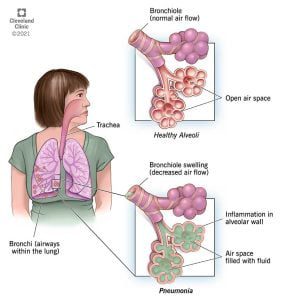
Pneumonia is a breathing condition in which there is inflammation (swelling) or an infection of the lungs or large airways.
Aspiration pneumonia occurs when food, saliva, liquids, or vomit is breathed into the lungs or airways leading to the lungs, instead of being swallowed into the esophagus and stomach.
As you can imagine, aspirating is a scary situation, especially for someone with an increased risk of choking. At The Arc of Monroe, our training surrounding food safety is of utmost importance for staff, especially when supporting people with developmental disabilities who have trouble chewing and/or swallowing.
Conditions in people with a developmental disability that increase the risk of aspiration include:
- Decreased or absent gag reflex
- Weakness of the muscles that are used in chewing and swallowing
- Gastro-esophageal Reflux Disease (GERD)
- Seizure disorder
- Eating too fast or having too much food in the mouth while eating
- Poor positioning during meals
- Medication side effects that relax the muscles used for chewing and swallowing
How can you help prevent aspiration pneumonia?
You can take a number of precautions to avoid aspiration pneumonia including:
- Always follow dietary guidelines.
- Keep the person you’re supporting upright when he or she is eating.
- Cut food into appropriately sized pieces.
- Encourage the person you’re supporting to chew slowly and completely.
- Notify the person’s healthcare provider if you notice any difficulty swallowing so they can make personalized recommendations to potentially change or adjust his or her diet or medication. They can also order tests or refer the patient to a speech or swallowing specialist.
- Make sure the person you’re supporting practices good oral hygiene.
How can you help someone with aspiration pneumonia?
Look for symptoms in the people you support:
- Shortness of breath (dyspnea) or wheezing.
- Coughing up blood or pus.
- Chest pain.
- Bad breath.
- Extreme tiredness.
Help the person you’re supporting get to their primary care physician for a physical exam. If the doctor can’t identify anything alarming right away, he or she may be able to assist through coordinating tests such as:
- Chest X-ray and/or a CT scan
- Blood tests
- Sputum tests
- Bronchoscopy
- Swallowing studies
With the right treatment, people with aspiration pneumonia often recover quickly and find they are feeling better after about a week. A doctor may recommend antibiotics depending on the kind of pneumonia and the patient’s medical history. In rare, extreme cases, additional treatment might include oxygen therapy or mechanical ventilation. Ultimately, each treatment plan should be tailored for the individual.
“It’s important to know the signs and symptoms of aspiration pneumonia, especially when supporting someone who is at a higher risk of choking and developing an infection,” Sue Sproule, Director of Nursing at The Arc of Monroe said. “Monitoring the size of food pieces, paying close attention at meal time, and recognizing when someone experiences aspiration could save a life.”
We hope this blog about aspiration pneumonia is helpful to you! Our Health Services team at The Arc of Monroe is a wealth of information. Our staff is made up of experienced professionals who primarily support people with disabilities. To learn more about who they are, visit our Health Services page. If you’re interested in working with us at The Arc of Monroe, visit our careers page. If you’d like to give and help make valuable resources like this possible, you can give online.

Sue Sproule is the Director of Nursing at The Arc of Monroe. She has 44 years of experience in nursing and four have been at The Arc of Monroe. To connect with Sue, email her at ssproule@arcmonroe.org.
Sources: